Ergonomic Training: How It Can Improve Your Health and Productivity
Ergonomic training is a critical component of workplace safety and overall health and wellness. It involves educating individuals on proper body mechanics, posture, and equipment use to reduce the risk of injury and improve productivity. The goal of ergonomic training is to optimize the interaction between workers and their environment, which can lead to numerous benefits for both the individual and the organization.
One of the primary benefits of ergonomic training is the prevention of workplace injuries. According to the National Safety Council, workplace injuries cost US businesses over $170 billion annually, and ergonomic-related injuries account for a significant portion of these costs. By educating workers on proper ergonomics, organizations can reduce the risk of injury and lower healthcare costs associated with workplace injuries.
Another benefit of ergonomic training is improved productivity. When individuals have the proper knowledge and tools to optimize their work environment, they can work more efficiently and with less fatigue. This leads to increased productivity, which can benefit both the individual and the organization.
In addition to the benefits within the workplace, ergonomic training can also improve overall health and wellness. By developing good habits and maintaining proper posture and body mechanics, individuals can reduce the risk of chronic pain and other musculoskeletal disorders. This can lead to improved quality of life and decreased healthcare costs associated with these conditions.
Overall, ergonomic training is a critical component of workplace safety and overall health and wellness. By optimizing the interaction between workers and their environment, organizations can reduce the risk of workplace injuries, increase productivity, and improve overall health and wellness.
The Importance of Ergonomics in the Workplace
The importance of ergonomics in the workplace cannot be overstated. Ergonomic training can significantly improve workplace safety and productivity, benefiting both the worker and the organization.

Workplace injuries are a major concern for organizations, and they can have significant financial and human costs. According to the Bureau of Labor Statistics, over 900,000 workplace injuries and illnesses resulted in time away from work in 2019 alone. These injuries can result in lost wages, medical expenses, and decreased productivity. In fact, a study by Liberty Mutual found that the most disabling workplace injuries cost US businesses $59 billion in 2019.
Ergonomic training can help prevent workplace injuries by teaching workers proper body mechanics, posture, and equipment use. By reducing the risk of injury, organizations can save money on workers’ compensation claims, medical expenses, and lost productivity.
In addition to improving workplace safety, ergonomic training can also increase productivity. When workers have the knowledge and tools to optimize their work environment, they can work more efficiently and with less fatigue. This can lead to increased productivity, improved quality of work, and increased job satisfaction.
Overall, the importance of ergonomic training in the workplace cannot be understated. By improving workplace safety and productivity, organizations can benefit both the worker and the organization. With the prevalence and cost of workplace injuries, ergonomic training is a critical investment for any organization that prioritizes the health and safety of their employees.
Common Workplace Hazards
There are several common workplace hazards that ergonomic training can help prevent. These hazards can lead to injuries and decreased productivity, making them a significant concern for organizations.
One of the most common workplace hazards is repetitive motion injuries. These injuries occur when workers perform the same motion repeatedly, leading to strain on the muscles, tendons, and nerves. Examples of repetitive motion injuries include carpal tunnel syndrome and tennis elbow. Ergonomic training can teach workers how to perform their tasks with less strain on their bodies, reducing the risk of repetitive motion injuries.
Another common workplace hazard is manual lifting and handling. Lifting heavy objects or performing repetitive lifting tasks can lead to strains and sprains. These injuries can be prevented by teaching workers proper lifting techniques and providing ergonomic lifting equipment, such as lift assists and adjustable height workstations.
Poor posture is another hazard that can lead to injuries and decreased productivity. When workers sit or stand in awkward positions for long periods, it can lead to pain and discomfort. Over time, poor posture can lead to chronic pain and musculoskeletal disorders. Ergonomic training can teach workers how to maintain proper posture and body mechanics, reducing the risk of injury and improving overall comfort.
Other common workplace hazards that ergonomic training can help prevent include slips, trips, and falls, exposure to vibration, and awkward or cramped workspaces. By educating workers on how to identify and prevent these hazards, organizations can improve workplace safety and productivity.
Overall, ergonomic training can help prevent several common workplace hazards that can lead to injuries and decreased productivity. By teaching workers how to perform their tasks with less strain on their bodies and how to maintain proper posture and body mechanics, organizations can create a safer and more comfortable work environment for their employees.
Proper Posture and Body Mechanics
Proper posture and body mechanics are critical components of ergonomic training. They can help prevent injuries and improve overall comfort and productivity in the workplace.
Maintaining proper posture is important because it helps distribute the weight of the body evenly and reduces the strain on muscles and joints. When workers sit or stand in awkward positions for long periods, it can lead to pain and discomfort. Over time, poor posture can lead to chronic pain and musculoskeletal disorders.
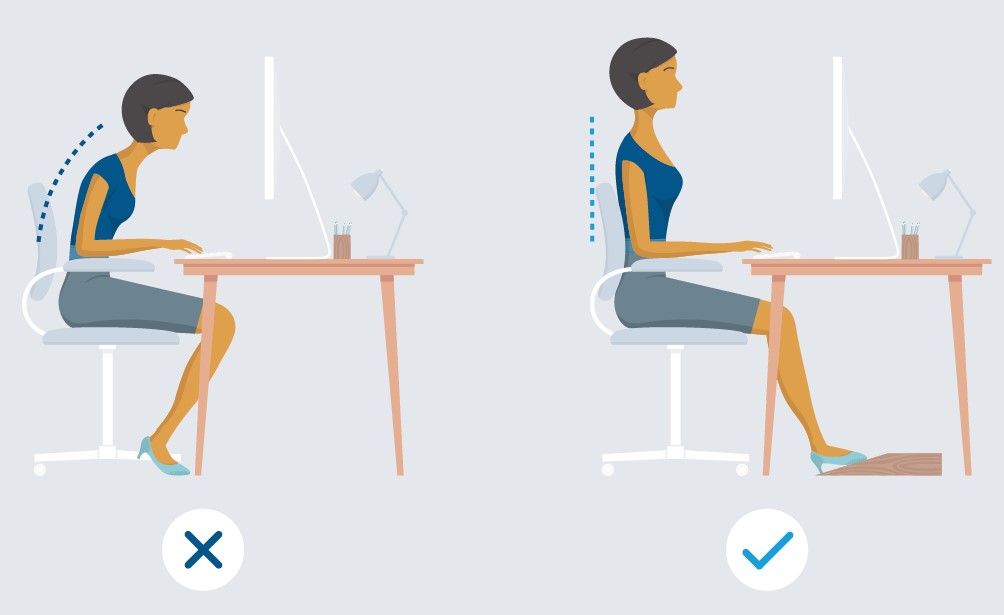
To maintain good posture, workers should keep their feet flat on the ground and their back straight. When sitting, they should use a chair with proper lumbar support and adjust the height so that their knees are level with their hips. Workers who stand for long periods should wear comfortable shoes with good arch support and shift their weight from one foot to the other regularly.
Body mechanics also play an important role in preventing injuries. Workers should use the largest muscles in their body to perform tasks, rather than relying on smaller muscles. For example, when lifting heavy objects, workers should use their legs to lift, rather than bending at the waist and using their back muscles.
To maintain good body mechanics, workers should keep their body aligned and avoid twisting or reaching when performing tasks. They should also avoid overreaching or bending their neck or back for extended periods. When working at a computer, workers should position the monitor so that the top of the screen is at or below eye level and the keyboard is at a comfortable distance from the body.
Overall, proper posture and body mechanics are essential for maintaining a healthy and comfortable work environment. By teaching workers how to maintain good posture and body mechanics, organizations can reduce the risk of injuries and improve overall productivity.
Equipment and Workstation Setup
Equipment and workstation setup are critical components of ergonomic training. The way equipment is arranged and used can significantly affect the ergonomics of a work environment.
Equipment that is poorly designed or adjusted can lead to awkward postures, excessive force, and repetitive motions. This can lead to pain and discomfort in the muscles and joints, as well as an increased risk of injury. On the other hand, equipment that is designed with ergonomics in mind can help prevent these problems and improve productivity.
When setting up a workstation, workers should make sure that the equipment is adjusted to fit their body size and shape. For example, the height of the chair, desk, and computer monitor should be adjustable to accommodate workers of different heights. The keyboard and mouse should be positioned so that the worker’s wrists are straight and their arms are relaxed.
Ergonomic equipment can also help improve posture and reduce the risk of injury. Examples of ergonomic equipment include ergonomic chairs, adjustable height workstations, and ergonomic keyboards and mice. When selecting ergonomic equipment, it is important to consider the individual needs of workers and choose equipment that fits their body size and shape.
Other tips for setting up a workstation and selecting ergonomic equipment include using document holders to reduce neck and eye strain, positioning the phone so that it is easy to reach, and using footrests to reduce pressure on the feet and legs. By paying attention to equipment and workstation setup, workers can improve their posture, reduce the risk of injury, and work more comfortably and productively.
Overall, equipment and workstation setup play a crucial role in ergonomics. By teaching workers how to set up their workstations and select ergonomic equipment, organizations can create a more comfortable and productive work environment.
Stretching and Exercise
Stretching and exercise are important components of ergonomic training. They can help improve flexibility, reduce the risk of injury, and increase overall comfort and productivity in the workplace.
Stretching can help prevent injuries by increasing flexibility and reducing muscle tension. When muscles are tight and inflexible, they are more susceptible to strain and injury. Stretching can help improve range of motion and reduce the risk of injury by loosening tight muscles and improving blood flow.
Examples of stretching exercises that can be incorporated into the workday include shoulder rolls, neck stretches, and wrist and finger stretches. These exercises can help reduce tension in the upper body and prevent repetitive motion injuries. They can also be done at a desk or workstation, making them easy to incorporate into the workday.
Exercise is also important for maintaining good health and preventing injuries. Regular exercise can help improve strength, flexibility, and endurance, which can all contribute to improved ergonomics and reduced risk of injury. Examples of exercises that can be incorporated into the workday include walking meetings, desk exercises, and standing desks.
Walking meetings involve taking a walk with colleagues rather than sitting in a conference room. Desk exercises, such as leg lifts or desk pushups, can be done during breaks or when transitioning between tasks. Standing desks allow workers to alternate between sitting and standing, which can help reduce the risk of injury from prolonged sitting.
Overall, stretching and exercise are essential components of ergonomic training. By incorporating stretching and exercise into the workday, workers can improve flexibility, reduce the risk of injury, and increase overall comfort and productivity.
Ergonomics Beyond the Workplace
Ergonomic habits can benefit overall health and wellness beyond the workplace. By incorporating ergonomic habits into daily life, individuals can reduce the risk of chronic pain and other musculoskeletal disorders, improve posture, and increase overall comfort and productivity.
One example of an ergonomic habit that can be incorporated into daily life is maintaining proper posture while sitting, standing, and walking. This can help reduce the risk of back pain, neck pain, and other musculoskeletal disorders. Additionally, regular exercise can help improve strength and flexibility, which can contribute to improved posture and reduced risk of injury.
Another example of an ergonomic habit is using proper lifting techniques when performing household tasks, such as lifting heavy objects or carrying groceries. Using the legs rather than the back to lift can help reduce the risk of injury and strain.
Other ergonomic habits to incorporate into daily life include taking frequent breaks when performing tasks that require prolonged sitting or standing, using a headset when talking on the phone to reduce neck and shoulder strain, and adjusting the height of computer monitors to reduce eye strain.
By incorporating ergonomic habits into daily life, individuals can improve overall health and wellness. These habits can help reduce the risk of chronic pain and musculoskeletal disorders, increase comfort and productivity, and improve overall quality of life.
Overall, ergonomics extends beyond the workplace and can benefit individuals in all areas of their lives. By incorporating ergonomic habits into daily life, individuals can improve their health and wellness and reduce the risk of injury and chronic pain.
Getting Started with Ergonomic Training
Getting started with ergonomic training can seem daunting, but it is an important investment in overall health and wellness. Here are some tips for getting started with ergonomic training and developing and maintaining ergonomic habits:
- Start with an ergonomic assessment: An ergonomic assessment can help identify areas of your workspace or daily routine that may be contributing to discomfort or injury. This can provide a starting point for making changes to improve ergonomics.
- Educate yourself: Learning about ergonomics and how to maintain proper posture and body mechanics is a critical first step in ergonomic training. There are many resources available, including online courses, books, and videos.
- Make changes gradually: It can be overwhelming to try to make all ergonomic changes at once. Start by making small changes, such as adjusting the height of your chair or taking more frequent breaks, and gradually build on these changes over time.
- Use ergonomic equipment: Ergonomic equipment, such as chairs, keyboards, and mice, can help reduce the risk of injury and improve comfort. Consider investing in ergonomic equipment that is appropriate for your needs.
- Incorporate stretching and exercise: Stretching and exercise can help improve flexibility, reduce muscle tension, and prevent injuries. Incorporate stretching and exercise into your daily routine to improve ergonomics and overall health and wellness.
- Be mindful of your body: Pay attention to your body and how it feels throughout the day. Take breaks and make adjustments as needed to maintain good posture and prevent discomfort or injury.
Overall, developing and maintaining ergonomic habits takes time and effort, but it is an important investment in overall health and wellness. By starting with an ergonomic assessment, educating yourself, making changes gradually, using ergonomic equipment, incorporating stretching and exercise, and being mindful of your body, you can improve ergonomics and reduce the risk of injury and chronic pain.
Conclusion
In conclusion, ergonomic training is a critical investment in workplace safety and overall health and wellness. By teaching workers how to maintain proper posture and body mechanics, use ergonomic equipment, and incorporate stretching and exercise into their daily routines, organizations can reduce the risk of injury and improve productivity.
The benefits of ergonomic training extend beyond the workplace and can improve overall health and wellness. By incorporating ergonomic habits into daily life, individuals can reduce the risk of chronic pain and other musculoskeletal disorders, improve posture, and increase overall comfort and productivity.
It is important to start small and make changes gradually, as developing and maintaining ergonomic habits takes time and effort. By starting with an ergonomic assessment, educating yourself, using ergonomic equipment, and incorporating stretching and exercise into your daily routine, you can improve ergonomics and reduce the risk of injury and chronic pain.
In conclusion, ergonomic training is an investment in your health and well-being. By incorporating ergonomic habits into daily life, you can improve posture, reduce the risk of injury, and increase overall comfort and productivity. So start today and make small changes that will lead to significant improvements in your health and well-being.
Acupuncture for Modern Pain Management | Traditional Chinese Medicine
Acupuncture is a traditional Chinese medicine practice that has been around for thousands of years. It involves inserting thin needles into specific points on the body to stimulate energy flow and promote healing. Over time, acupuncture has evolved into a modern-day treatment that is used to manage a variety of health conditions, including pain.
The history of acupuncture can be traced back to ancient China, where it was first used as a form of traditional medicine. According to Chinese philosophy, the human body is made up of channels or meridians through which energy flows. When these channels become blocked or disrupted, it can lead to illness and pain. Acupuncture was developed as a way to restore the balance of energy in the body and promote healing.
Today, acupuncture has gained widespread acceptance as a complementary and alternative therapy for various conditions, including chronic pain, headaches, and migraines, among others. The purpose of this article is to explore the benefits of acupuncture for modern pain management, including its effectiveness in treating chronic pain, headaches, back pain, joint pain, anxiety, and depression. We will also discuss tips for finding a qualified acupuncturist and maintaining good habits for pain management.
Acupuncture for Pain Relief
Acupuncture works for pain relief by stimulating specific points on the body that correspond to the site of pain. The stimulation of these points helps to release endorphins, which are natural painkillers produced by the body. Additionally, acupuncture promotes the release of other substances that help to reduce inflammation and promote healing.

Numerous studies have shown acupuncture to be effective in treating various types of pain, including chronic pain, headaches, back pain, and joint pain. In fact, the National Center for Complementary and Integrative Health (NCCIH) has recognized acupuncture as an effective treatment for several types of pain.
One study published in the Archives of Internal Medicine found that acupuncture was effective in relieving chronic pain, including back pain and osteoarthritis. Another study published in the Journal of Pain found that acupuncture was effective in reducing the frequency and intensity of tension headaches.
A review of 29 studies conducted by the Cochrane Collaboration found that acupuncture was effective in treating chronic low back pain. The review also found that acupuncture was more effective than conventional treatments such as medication and physical therapy.
Overall, these studies and many others suggest that acupuncture is an effective and safe treatment option for various types of pain. If you are considering acupuncture for pain relief, it is important to find a qualified acupuncturist who can help you develop a personalized treatment plan.
Acupuncture for Chronic Pain
Chronic pain is defined as pain that lasts for more than 12 weeks or persists beyond the time of normal tissue healing. It is estimated that chronic pain affects over 100 million adults in the United States and is a leading cause of disability and lost productivity.

Studies have shown that acupuncture can be an effective treatment option for chronic pain. A 2012 study published in the Archives of Internal Medicine found that acupuncture was effective in reducing chronic pain by about 50%. The study also found that acupuncture was more effective than traditional pain management options such as medication.
Another study published in the Journal of Pain Research found that acupuncture was effective in reducing pain and improving quality of life in patients with chronic pain conditions such as fibromyalgia, chronic low back pain, and chronic neck pain.
One advantage of acupuncture over traditional pain management options such as medication is that it is generally considered safe and has few side effects. Medications used to treat chronic pain can have serious side effects, including addiction and overdose.
However, it is important to note that acupuncture may not work for everyone, and its effectiveness may depend on the individual and the type of pain being treated. In some cases, a combination of acupuncture and other pain management techniques may be necessary for optimal results.
In summary, acupuncture is a safe and effective treatment option for chronic pain, and it may be a good alternative to traditional pain management options such as medication. If you are considering acupuncture for chronic pain, it is important to work with a qualified acupuncturist to develop a personalized treatment plan.
Acupuncture for Headaches and Migraines
Headaches and migraines can have a significant impact on an individual’s quality of life. They can cause debilitating pain, sensitivity to light and sound, nausea, and vomiting. For those who suffer from chronic headaches or migraines, it can be difficult to carry out daily activities and maintain productivity.
Acupuncture has been found to be an effective treatment option for headaches and migraines. It works by stimulating specific points on the body that are believed to be associated with pain relief. Acupuncture can also help to reduce stress and tension, which can trigger headaches and migraines.
Several studies have demonstrated the effectiveness of acupuncture for treating headaches and migraines. One study published in the Journal of the American Medical Association found that acupuncture was effective in reducing the frequency and intensity of migraines.
Another study published in the Cochrane Database of Systematic Reviews found that acupuncture was effective in reducing the frequency and intensity of tension headaches. The study also found that acupuncture had fewer side effects compared to traditional headache medications.
Overall, these studies and others suggest that acupuncture can be an effective and safe treatment option for headaches and migraines. If you are considering acupuncture for headache or migraine relief, it is important to work with a qualified acupuncturist who can help you develop a personalized treatment plan.
Acupuncture for Back Pain
Back pain is a common condition that affects millions of people in the United States. It can range from mild discomfort to debilitating pain that interferes with daily activities. Back pain can be caused by a variety of factors, including injury, poor posture, and degenerative conditions.
Acupuncture has been found to be an effective treatment option for back pain. It works by stimulating specific points on the body that are believed to be associated with pain relief and promoting the body’s natural healing process.
Several studies have demonstrated the effectiveness of acupuncture for treating back pain. A study published in the Journal of the American Medical Association found that acupuncture was effective in reducing chronic low back pain.
Another study published in the Annals of Internal Medicine found that acupuncture was more effective than conventional treatments such as medication and physical therapy for reducing chronic low back pain.
A review of 33 studies published in the Journal of Pain found that acupuncture was effective in reducing back pain and improving overall function in patients with chronic back pain.
Overall, these studies and others suggest that acupuncture can be an effective and safe treatment option for back pain. If you are considering acupuncture for back pain relief, it is important to work with a qualified acupuncturist who can help you develop a personalized treatment plan.
Acupuncture for Joint Pain
Joint pain is a common condition that affects millions of people in the United States. It can be caused by a variety of factors, including injury, overuse, and arthritis. Joint pain can be debilitating and interfere with daily activities.
Acupuncture has been found to be an effective treatment option for joint pain. It works by stimulating specific points on the body that are believed to be associated with pain relief and promoting the body’s natural healing process.
Several studies have demonstrated the effectiveness of acupuncture for treating joint pain. A review of 43 studies published in the Clinical Journal of Pain found that acupuncture was effective in reducing pain and improving physical function in patients with knee osteoarthritis.
Another study published in the Annals of Internal Medicine found that acupuncture was effective in reducing pain and improving function in patients with osteoarthritis of the knee.
A review of 18 studies published in the Journal of Pain found that acupuncture was effective in reducing pain and improving function in patients with chronic pain conditions, including joint pain.
Overall, these studies and others suggest that acupuncture can be an effective and safe treatment option for joint pain. If you are considering acupuncture for joint pain relief, it is important to work with a qualified acupuncturist who can help you develop a personalized treatment plan.
Acupuncture for Anxiety and Depression
Anxiety and depression are common mental health conditions that can have a significant impact on an individual’s quality of life. They can cause persistent feelings of sadness, hopelessness, and anxiety, making it difficult to carry out daily activities.
Acupuncture has been found to be an effective treatment option for anxiety and depression. It works by stimulating specific points on the body that are believed to be associated with the regulation of emotions and the release of endorphins, which are natural mood boosters.
Several studies have demonstrated the effectiveness of acupuncture for treating anxiety and depression. A review of 10 studies published in the Journal of Affective Disorders found that acupuncture was effective in reducing symptoms of depression.
Another study published in the Journal of Alternative and Complementary Medicine found that acupuncture was effective in reducing anxiety and depression symptoms in women with postpartum depression.
A review of 20 studies published in the Journal of Evidence-Based Complementary and Alternative Medicine found that acupuncture was effective in reducing symptoms of anxiety.
Overall, these studies and others suggest that acupuncture can be an effective and safe treatment option for anxiety and depression. If you are considering acupuncture for anxiety or depression relief, it is important to work with a qualified acupuncturist who can help you develop a personalized treatment plan.
Choosing an Acupuncturist
Choosing the right acupuncturist is an important part of receiving effective acupuncture treatment. Here are some tips for finding a qualified acupuncturist:
- Look for licensed and certified practitioners: Acupuncturists in the United States should be licensed by the state in which they practice and certified by the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM).
- Check for experience and training: Look for acupuncturists who have experience and training in treating the specific condition you are seeking treatment for.
- Read reviews and ask for referrals: Read online reviews and ask for referrals from friends and family who have had acupuncture treatment.
- Consider the practitioner’s bedside manner: Choose an acupuncturist who makes you feel comfortable and who takes the time to listen to your concerns.
Establishing a good patient-practitioner relationship is also important for effective acupuncture treatment. This relationship involves trust, communication, and mutual respect.
During an acupuncture treatment, the acupuncturist will insert thin needles into specific points on your body. You may feel a slight prick or pressure, but the needles should not cause pain. You will typically lie still for 15-30 minutes with the needles in place.
After the treatment, you may feel relaxed or energized. It is important to drink plenty of water and avoid strenuous activity for a few hours after the treatment.
Overall, acupuncture can be a safe and effective treatment option for various conditions, but it is important to work with a qualified acupuncturist and establish a good patient-practitioner relationship for the best results.
Maintaining Good Habits for Pain Management
In addition to receiving acupuncture treatment, there are several lifestyle habits that can support pain management and enhance the benefits of acupuncture. Here are some tips for developing and maintaining these habits:
- Exercise regularly: Regular exercise can help to reduce pain, improve mobility, and promote overall health. It is important to choose exercises that are appropriate for your condition and fitness level, and to consult with your healthcare provider before starting a new exercise program.
- Maintain a healthy diet: A healthy diet that is rich in fruits, vegetables, lean protein, and whole grains can help to reduce inflammation and support overall health. It is important to avoid foods that may trigger inflammation, such as processed foods and sugary drinks.
- Practice stress management techniques: Stress can exacerbate pain and other health conditions. Techniques such as meditation, deep breathing, and yoga can help to reduce stress and promote relaxation.
- Get enough sleep: Sleep is important for overall health and can help to reduce pain and inflammation. It is important to establish good sleep habits, such as sticking to a regular sleep schedule and avoiding screens before bedtime.
Developing and maintaining these habits can be challenging, but there are several tips that can help:
- Set realistic goals: Start with small goals and work your way up. It is important to be patient and consistent in order to see results.
- Find activities that you enjoy: Exercise and other healthy habits are more likely to become a part of your routine if you enjoy them.
- Seek support: Enlist the help of friends, family members, or a healthcare provider to help you develop and maintain healthy habits.
- Keep a journal: Keeping a journal can help you track your progress and identify areas for improvement.
In summary, developing and maintaining healthy habits can support pain management and enhance the benefits of acupuncture treatment. It is important to consult with your healthcare provider and work with a qualified acupuncturist to develop a comprehensive pain management plan.
Conclusion
Acupuncture is a safe and effective treatment option for modern pain management. It has been found to be effective in treating chronic pain, headaches and migraines, back pain, joint pain, and even anxiety and depression. Acupuncture works by stimulating specific points on the body that are associated with pain relief and promoting the body’s natural healing process.
If you are suffering from pain, it is important to explore acupuncture as a treatment option. Working with a qualified acupuncturist and developing healthy lifestyle habits can help to support pain management and enhance the benefits of acupuncture treatment.
It is also important to take a holistic approach to pain management, which may include a combination of acupuncture, medication, physical therapy, and other therapies. By working with your healthcare provider and taking a comprehensive approach, you can find the right combination of treatments to manage your pain and improve your overall quality of life.
Can Exercise Therapy Help Manage Chronic Pain? Benefits & Tips
Chronic pain is a complex and challenging condition that affects millions of people worldwide. It can have a significant impact on an individual’s quality of life, making it difficult to perform daily tasks and participate in activities they enjoy. For many people with chronic pain, finding an effective solution can be a long and frustrating journey.
One potential solution that has gained increasing attention in recent years is exercise therapy. Exercise therapy involves a range of physical activities designed to improve strength, flexibility, and overall physical function. It has been shown to be effective in managing a wide variety of health conditions, including chronic pain.
In this article, we will explore the question of whether exercise therapy can help manage chronic pain. We will examine the benefits of exercise therapy, cite relevant studies, and offer tips for developing and maintaining an exercise routine. By the end of this article, you will have a better understanding of how exercise therapy can be an effective tool in managing chronic pain.
What is Chronic Pain?
Before delving into how exercise therapy can help manage chronic pain, it’s important to define what we mean by chronic pain and understand its causes.
Chronic pain is pain that persists for an extended period, typically longer than three months. Unlike acute pain, which is a normal bodily response to injury or tissue damage, chronic pain is often not directly related to any injury or underlying medical condition.
There are many potential causes of chronic pain, including conditions such as arthritis, fibromyalgia, and neuropathy, as well as previous injuries or surgeries. In some cases, chronic pain may have no clear cause and be classified as “chronic non-specific pain.”
Regardless of the cause, chronic pain can have a significant impact on an individual’s physical and emotional well-being, leading to decreased activity levels, poor sleep, anxiety, and depression. It is important to manage chronic pain effectively to prevent these negative outcomes and improve overall quality of life.
How Exercise Therapy Can Help
Exercise therapy is a promising approach to managing chronic pain. Research has shown that regular physical activity can help alleviate pain symptoms and improve physical function. Here are some of the benefits of exercise therapy for managing chronic pain:
- Reduced pain intensity: Exercise has been shown to reduce pain intensity in people with chronic pain. Regular physical activity helps to release endorphins, the body’s natural painkillers, which can help to alleviate pain symptoms.
- Improved physical function: Chronic pain can make it difficult to perform daily tasks and participate in activities. Exercise therapy can improve strength, flexibility, and overall physical function, making it easier for individuals with chronic pain to perform activities of daily living.
- Reduced reliance on medication: Exercise therapy can help reduce reliance on medication for pain management. This is particularly important given the potential side effects of pain medications, including addiction, tolerance, and gastrointestinal problems.
- Improved mental health: Chronic pain can have a significant impact on an individual’s mental health, leading to anxiety and depression. Exercise therapy has been shown to improve mood and reduce symptoms of anxiety and depression.
When it comes to the types of exercises that can be beneficial for chronic pain sufferers, there is no one-size-fits-all approach. However, some types of exercise that have been shown to be particularly helpful include:
- Aerobic exercise: Aerobic exercise, such as walking, cycling, or swimming, can help improve cardiovascular health, reduce pain symptoms, and increase overall physical function.
- Strength training: Strength training exercises, such as weightlifting or resistance band exercises, can help build muscle mass and improve overall physical function.
- Stretching: Stretching exercises, such as yoga or Pilates, can help improve flexibility and reduce pain symptoms.
It is important to note that exercise therapy should be tailored to the individual and their specific needs and abilities. Working with a physical therapist or other qualified healthcare professional can help ensure that the exercise therapy program is safe and effective.
Studies on Exercise Therapy and Chronic Pain
Numerous studies have investigated the effectiveness of exercise therapy for managing chronic pain. Here are a few examples of studies that support the use of exercise therapy:
- A systematic review and meta-analysis published in the Journal of Pain in 2017 found that exercise therapy is effective in reducing pain intensity and improving physical function in people with chronic low back pain. The review analyzed 23 randomized controlled trials involving over 2,600 participants.
- A randomized controlled trial published in the Annals of Internal Medicine in 2016 found that a 12-week exercise program consisting of aerobic exercise and resistance training was effective in reducing pain intensity and improving physical function in older adults with knee osteoarthritis.
- A randomized controlled trial published in JAMA Internal Medicine in 2018 found that a 12-week exercise program consisting of aerobic exercise and resistance training was effective in reducing pain intensity and improving physical function in people with fibromyalgia.
Overall, these studies and others have consistently found that exercise therapy is an effective tool for managing chronic pain. Exercise therapy can help reduce pain intensity, improve physical function, and enhance overall quality of life for individuals with chronic pain.
Working with a Physical Therapist
Working with a physical therapist can be an effective way to develop an exercise therapy plan for managing chronic pain. A physical therapist is a healthcare professional who is trained to assess, diagnose, and treat movement-related conditions, including chronic pain.
Here’s how a physical therapist can help someone with chronic pain develop an exercise therapy plan:
- Assessment: The physical therapist will conduct an initial assessment to evaluate the individual’s pain symptoms, medical history, and physical function. This assessment will help the physical therapist develop an individualized exercise therapy plan that is tailored to the individual’s specific needs and abilities.
- Goal setting: The physical therapist will work with the individual to set realistic goals for their exercise therapy plan. Goals may include reducing pain symptoms, improving physical function, or increasing overall activity levels.
- Exercise selection: The physical therapist will select exercises that are appropriate for the individual’s specific needs and abilities. Exercises may include aerobic exercise, strength training, stretching, or a combination of these.
- Instruction: The physical therapist will provide instruction on how to perform the exercises safely and effectively. This may include demonstrating the exercises and providing feedback on form and technique.
- Progression: The physical therapist will monitor the individual’s progress and adjust the exercise therapy plan as needed. This may include increasing the intensity or duration of exercises as the individual’s physical function improves.
Working with a physical therapist can help ensure that the exercise therapy plan is safe, effective, and tailored to the individual’s specific needs and abilities. It is important to follow the physical therapist’s recommendations and guidance closely to achieve the best possible outcomes.
Tips for Developing an Exercise Routine
Developing a successful exercise routine can be a key component of managing chronic pain. Here are some tips for developing an exercise routine that can help manage chronic pain:
- Start slowly: It’s important to start slowly and gradually increase the intensity and duration of exercise over time. This can help prevent injury and minimize pain symptoms. Begin with low-intensity exercises and gradually increase the intensity as your physical function improves.
- Pacing: Pacing involves balancing periods of activity with periods of rest. This can help prevent overexertion and minimize pain symptoms. Plan your exercise routine with regular rest breaks and avoid pushing yourself too hard.
- Variety: Incorporate a variety of exercises into your routine to avoid boredom and prevent overuse injuries. Try a mix of aerobic exercise, strength training, and stretching.
- Consistency: Consistency is key when it comes to exercise therapy. Make exercise a regular part of your routine, and try to stick to a schedule.
- Listen to your body: It’s important to listen to your body and adjust your exercise routine as needed. If you experience pain or discomfort during exercise, adjust the intensity or type of exercise accordingly.
- Seek professional guidance: Working with a physical therapist or other qualified healthcare professional can be helpful in developing a safe and effective exercise routine. They can provide guidance on exercise selection, technique, and progression.
By following these tips, you can develop a successful exercise routine that can help manage chronic pain and improve physical function. Remember to start slowly, pace yourself, and listen to your body to achieve the best possible outcomes.
Tips for Maintaining an Exercise Routine
Maintaining an exercise routine for the long-term can be challenging, but it is an important component of managing chronic pain. Here are some tips for staying motivated and accountable when it comes to exercise therapy:
- Set realistic goals: Setting realistic goals can help you stay motivated and focused. Break your goals down into smaller, achievable steps and track your progress along the way.
- Find a workout buddy: Having a workout buddy can provide accountability and motivation. Consider finding a friend or family member to exercise with or join a group exercise class.
- Mix it up: Adding variety to your exercise routine can help prevent boredom and keep things interesting. Try new exercises or activities to keep things fresh.
- Use technology: There are many apps and wearable devices that can help track your exercise progress and provide motivation. Consider using a fitness tracker or exercise app to help you stay on track.
- Reward yourself: Rewarding yourself for reaching your exercise goals can provide motivation and a sense of accomplishment. Treat yourself to something you enjoy, like a massage or a favorite meal.
- Be flexible: Life can be unpredictable, and it’s important to be flexible when it comes to your exercise routine. If you miss a workout or have to adjust your schedule, don’t get discouraged. Just get back on track as soon as you can.
- Remember the benefits: Remind yourself of the benefits of exercise therapy, such as improved physical function, reduced pain symptoms, and better overall health. Keeping these benefits in mind can help you stay motivated and committed to your exercise routine.
By staying accountable and motivated, you can maintain an exercise routine for the long-term and reap the benefits of exercise therapy for managing chronic pain.
The Role of Diet and Lifestyle Factors
Diet and lifestyle factors can have a significant impact on chronic pain. Here’s how:
- Inflammation: Chronic pain is often associated with inflammation, and diet can play a role in reducing or exacerbating inflammation. A diet high in processed foods, sugar, and unhealthy fats can contribute to inflammation, while a diet rich in whole foods, fruits, vegetables, and healthy fats can help reduce inflammation.
- Weight management: Maintaining a healthy weight is important for managing chronic pain. Excess weight can put additional stress on joints and exacerbate pain symptoms.
- Physical activity: Regular physical activity is an important component of managing chronic pain, but it can be difficult to achieve without a healthy diet. Eating a balanced diet that provides the energy and nutrients needed for physical activity can help make exercise therapy more effective.
- Sleep: Chronic pain can disrupt sleep, which can in turn exacerbate pain symptoms. Making positive changes to diet and lifestyle habits, such as avoiding caffeine and alcohol before bed, can help improve sleep quality.
Here are some tips for making positive changes to diet and lifestyle habits to help manage chronic pain:
- Eat a balanced diet: Focus on a diet rich in whole foods, fruits, vegetables, and healthy fats. Avoid processed foods, sugar, and unhealthy fats.
- Maintain a healthy weight: Work with a healthcare professional to achieve and maintain a healthy weight through diet and exercise therapy.
- Stay active: Incorporate regular physical activity into your routine, with guidance from a physical therapist or healthcare professional.
- Manage stress: Stress can exacerbate pain symptoms. Find stress-management techniques that work for you, such as meditation or deep breathing exercises.
- Get enough sleep: Aim for 7-9 hours of sleep per night and make positive changes to your sleep environment and routine.
By making positive changes to diet and lifestyle habits, you can help manage chronic pain and improve overall health and well-being.
Other Pain Management Techniques
While exercise therapy can be an effective tool for managing chronic pain, it is often most effective when used in conjunction with other pain management techniques. Here are some other pain management techniques that can be used alongside exercise therapy:
- Medication: In some cases, medication may be necessary to manage chronic pain. There are many different types of pain medications available, including over-the-counter pain relievers, prescription medications, and opioid medications. It is important to work closely with a healthcare professional when using pain medications to minimize the risk of addiction, tolerance, and other negative side effects.
- Mind-body techniques: Mind-body techniques, such as meditation, yoga, and tai chi, can help reduce stress and promote relaxation, which can in turn reduce pain symptoms.
- Cognitive-behavioral therapy: Cognitive-behavioral therapy (CBT) is a type of talk therapy that can help individuals with chronic pain manage their thoughts and emotions related to pain. CBT can help individuals develop coping strategies and improve overall mental health.
- Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body. It has been shown to be effective in reducing pain symptoms in some individuals with chronic pain.
- Massage therapy: Massage therapy can help reduce muscle tension and promote relaxation, which can in turn reduce pain symptoms.
It is important to take a multi-faceted approach to managing chronic pain, incorporating a range of pain management techniques as appropriate. Working with a healthcare professional can help ensure that the pain management plan is safe and effective, and tailored to the individual’s specific needs and abilities.
Conclusion
Exercise therapy is a promising tool for managing chronic pain. It has been shown to reduce pain intensity, improve physical function, and enhance overall quality of life for individuals with chronic pain. Whether you’re living with chronic pain or supporting someone who is, exercise therapy can be an effective and safe option for pain management.
If you’re considering exercise therapy for chronic pain management, remember that it is important to work with a qualified healthcare professional to develop an individualized exercise plan that is tailored to your specific needs and abilities. It’s also important to take a multi-faceted approach to pain management, incorporating a range of techniques as appropriate.
With dedication, patience, and guidance from a healthcare professional, exercise therapy can be a powerful tool for managing chronic pain and improving overall physical and mental well-being. Don’t hesitate to reach out to a healthcare professional for guidance and support on your pain management journey.
Joint Mobilization vs. Manipulation: Understanding the Key Differences
When it comes to managing pain and improving joint function, joint mobilization and manipulation are two common techniques that healthcare providers may use. While the two terms may sound similar, there are important differences between them that are worth understanding.
Joint mobilization is a technique used to improve joint movement and function by applying gentle, passive movements to the affected joint. This technique can be used to treat a variety of conditions, such as arthritis, sprains, and strains. On the other hand, manipulation is a more forceful technique that involves the application of a high-velocity, low-amplitude thrust to the joint. This technique is often used to treat conditions such as back pain and neck pain.
Understanding the difference between joint mobilization and manipulation is crucial, as the appropriate technique depends on the individual patient’s needs and condition. In some cases, joint mobilization may be more appropriate, while in others, manipulation may be necessary. Moreover, it is important to seek treatment from a qualified healthcare provider who has experience in both techniques to ensure that the right approach is taken for your specific condition.
In the following sections, we will explore the benefits, techniques, conditions that can be treated, and potential risks associated with both joint mobilization and manipulation. We will also discuss how to choose the right treatment option and provide tips for maintaining healthy joints. By the end of this article, you will have a better understanding of the difference between joint mobilization and manipulation and how to make informed decisions about your joint health.
Joint Mobilization
Joint mobilization is a manual therapy technique used to improve joint mobility and function by gently moving the affected joint through its range of motion. The goal of joint mobilization is to reduce pain, restore joint movement, and improve overall function.

One of the key benefits of joint mobilization is that it is a non-invasive, non-surgical treatment option that can be used to treat a variety of conditions, such as arthritis, sports injuries, and post-surgical rehabilitation. Joint mobilization can also be used to prevent joint stiffness and immobility, especially in patients who are recovering from a prolonged period of immobilization.
There are various techniques used in joint mobilization, depending on the affected joint and the patient’s condition. Some techniques involve applying sustained pressure to the joint while others involve rhythmic oscillations or passive movements. A qualified healthcare provider will select the appropriate technique based on the patient’s needs and condition.
Research studies have shown that joint mobilization can be an effective treatment option for a range of conditions. For example, a study published in the Journal of Manipulative and Physiological Therapeutics found that joint mobilization can significantly reduce pain and improve joint function in patients with knee osteoarthritis. Another study published in the Journal of Orthopaedic and Sports Physical Therapy found that joint mobilization can improve shoulder function and reduce pain in patients with rotator cuff tendinopathy.
Overall, joint mobilization is a safe and effective treatment option for improving joint mobility, reducing pain, and improving overall function in patients with various conditions.
Manipulation
Manipulation is a manual therapy technique that involves applying a high-velocity, low-amplitude thrust to the affected joint. The goal of manipulation is to restore joint function, reduce pain, and improve overall physical function.
One of the key benefits of manipulation is that it can provide immediate relief from pain and improve joint function in a short amount of time. Manipulation can also be used to treat a variety of conditions, such as back pain, neck pain, and headaches. Additionally, manipulation can be used as a complementary therapy to other treatments, such as physical therapy and medication.
There are various techniques used in manipulation, including spinal manipulation, which involves applying a high-velocity, low-amplitude thrust to the spine, and extremity manipulation, which involves applying the same technique to the arms or legs. A qualified healthcare provider will select the appropriate technique based on the patient’s needs and condition.
Research studies have shown that manipulation can be an effective treatment option for a range of conditions. For example, a study published in the Annals of Internal Medicine found that spinal manipulation can provide significant relief from low back pain. Another study published in the Journal of Manipulative and Physiological Therapeutics found that manipulation can improve neck mobility and reduce pain in patients with neck pain.
Overall, manipulation is a safe and effective treatment option for improving joint function, reducing pain, and improving overall physical function in patients with various conditions. However, it is important to seek treatment from a qualified healthcare provider who has experience in manipulation to ensure that the technique is used appropriately and safely.
Comparison of Joint Mobilization and Manipulation
While joint mobilization and manipulation are both manual therapy techniques used to improve joint function and reduce pain, there are important differences between the two.
One of the key differences between joint mobilization and manipulation is the level of force applied to the affected joint. Joint mobilization involves applying gentle, passive movements to the joint, while manipulation involves applying a high-velocity, low-amplitude thrust to the joint. This means that manipulation may be more appropriate for conditions that require a higher level of force to restore joint function, such as back pain and neck pain.
Another difference between joint mobilization and manipulation is the technique used to perform the therapy. Joint mobilization involves a variety of techniques, including sustained pressure, rhythmic oscillations, and passive movements, while manipulation involves a quick, thrusting movement to the joint. Additionally, joint mobilization is typically performed by a physical therapist, while manipulation is usually performed by a chiropractor.
Despite these differences, there are also similarities between joint mobilization and manipulation. Both techniques are non-surgical, non-invasive treatment options that can be used to improve joint function and reduce pain. Moreover, the appropriate treatment option for a patient depends on various factors, including the patient’s age, medical history, and the severity of their condition.
Factors that may determine the appropriate treatment option include the patient’s pain level, the location of the affected joint, and the underlying cause of the condition. In general, joint mobilization may be more appropriate for patients with milder symptoms, while manipulation may be more appropriate for patients with severe pain and limited mobility.
Ultimately, the appropriate treatment option for a patient should be determined by a qualified healthcare provider who has experience in both joint mobilization and manipulation. It is important to discuss your individual needs and concerns with your provider to ensure that the most appropriate treatment option is selected for your specific condition.
Risks and Safety Concerns
While joint mobilization and manipulation are generally safe and effective treatment options, there are potential risks and safety concerns associated with both techniques.
One of the potential risks associated with joint mobilization is the possibility of aggravating an existing injury or condition. If the technique is performed improperly or without proper assessment of the patient’s condition, joint mobilization can cause pain or discomfort. Moreover, joint mobilization may not be appropriate for patients with certain conditions, such as fractures or dislocations.
Similarly, manipulation also carries some potential risks. The most common adverse effect of manipulation is soreness or discomfort in the affected joint or surrounding muscles. In rare cases, manipulation can cause more serious adverse effects, such as fractures or dislocations. Moreover, manipulation may not be appropriate for patients with certain conditions, such as osteoporosis or spinal cord injury.
To reduce the risks of adverse effects, it is important to seek treatment from a qualified healthcare provider who has experience in both joint mobilization and manipulation. The provider should assess the patient’s medical history, current condition, and any other relevant factors before recommending either technique. Additionally, patients should communicate any concerns or discomfort they experience during the treatment process to their provider.
Patients can also reduce the risks of adverse effects by following any post-treatment instructions provided by their healthcare provider. This may include avoiding certain activities or exercises, applying heat or ice to the affected area, or taking pain medication as prescribed.
Overall, joint mobilization and manipulation are safe and effective treatment options for improving joint function and reducing pain. However, patients should be aware of the potential risks and safety concerns associated with both techniques and should seek treatment from a qualified healthcare provider to minimize the risks of adverse effects.
How to Choose the Right Treatment
Choosing the right treatment option between joint mobilization and manipulation depends on several factors. Patients should consider the severity of their condition, their medical history, and any underlying medical conditions. They should also consider the potential benefits and risks associated with each treatment option.
The role of the healthcare provider is crucial in making the decision between joint mobilization and manipulation. A qualified healthcare provider can assess the patient’s medical history, current condition, and any other relevant factors to determine which technique is appropriate. The provider can also explain the potential benefits and risks associated with each technique, as well as answer any questions or concerns the patient may have.
To communicate their preferences and concerns to their healthcare provider, patients should be honest and open about their symptoms and expectations. They should ask any questions they may have about the treatment options and express any concerns they may have about the potential risks or discomfort associated with either technique. Patients should also be willing to follow the provider’s recommendations and ask for clarification if anything is unclear.
It is also important to consider the provider’s level of experience and expertise in both joint mobilization and manipulation. Patients should seek treatment from a qualified healthcare provider who has experience in both techniques to ensure that the most appropriate treatment option is selected for their specific condition.
In summary, patients should consider several factors when choosing between joint mobilization and manipulation, including the severity of their condition, their medical history, and any underlying medical conditions. The healthcare provider plays a crucial role in making the decision, and patients should communicate their preferences and concerns openly to ensure the most appropriate treatment option is selected.
Tips for Developing and Maintaining Healthy Joints
Maintaining healthy joints is important for overall physical function and quality of life. Here are some tips for developing and maintaining healthy joints:
- Exercise regularly: Regular exercise can help improve joint flexibility, strength, and overall function. Exercise can also help reduce the risk of joint-related conditions, such as osteoarthritis and rheumatoid arthritis.
- Maintain a healthy weight: Being overweight or obese can put extra stress on the joints, leading to joint pain and inflammation. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce the risk of joint-related conditions.
- Practice good posture: Poor posture can cause joint pain and discomfort, especially in the neck, back, and hips. Practicing good posture can help reduce the risk of joint pain and improve overall physical function.
- Avoid repetitive motions: Repetitive motions, such as typing or using a computer mouse, can cause joint pain and inflammation over time. Taking regular breaks and using ergonomic equipment can help reduce the risk of joint-related conditions.
- Wear appropriate footwear: Wearing appropriate footwear with good arch support can help reduce the risk of joint pain, especially in the feet, ankles, and knees.
- Stay hydrated: Drinking plenty of water can help keep the joints lubricated and reduce the risk of joint pain and stiffness.
- Take breaks and rest: Taking regular breaks and resting when needed can help prevent joint overuse and reduce the risk of joint-related conditions.
Overall, lifestyle modifications such as regular exercise, maintaining a healthy weight, practicing good posture, and avoiding repetitive motions can help improve joint health and reduce the risk of joint-related conditions. Additionally, seeking treatment from a qualified healthcare provider when experiencing joint pain or discomfort can help prevent further damage and improve overall function.
Conclusion
In summary, joint mobilization and manipulation are both manual therapy techniques used to improve joint function and reduce pain, but there are important differences between the two. Joint mobilization involves applying gentle, passive movements to the joint, while manipulation involves applying a high-velocity, low-amplitude thrust to the joint. The appropriate treatment option depends on several factors, including the patient’s condition and medical history.
It is important to seek professional advice before undergoing joint mobilization or manipulation to ensure that the most appropriate treatment option is selected for your specific condition. A qualified healthcare provider can assess your medical history, current condition, and any other relevant factors to determine which technique is appropriate.
In addition to seeking professional advice, lifestyle modifications such as regular exercise, maintaining a healthy weight, and practicing good posture can help improve joint health and reduce the risk of joint-related conditions.
In conclusion, joint mobilization and manipulation are safe and effective treatment options for improving joint function and reducing pain. Patients should seek treatment from a qualified healthcare provider, communicate their preferences and concerns openly, and follow any post-treatment instructions to ensure the best possible outcome.
How Home Physiotherapy Can Help You Recover Faster After Injury | Benefits, Exercises & More
After an injury, it is common to experience pain, stiffness, and reduced mobility. Recovering from an injury can be a lengthy and frustrating process, but the good news is that there are ways to speed up the recovery process. One effective method is home physiotherapy.
Home physiotherapy is a form of physical therapy that can be performed in the comfort of your own home. It involves a variety of exercises, stretches, and movements that are designed to help you recover from an injury and improve your overall physical function.
The benefits of home physiotherapy are numerous. Not only is it a cost-effective alternative to in-clinic physiotherapy, but it also provides the convenience of being able to perform exercises in your own familiar surroundings. In this article, we will explore the importance of recovering faster after an injury and how home physiotherapy can help you achieve that goal.
Understanding Physiotherapy
Physiotherapy, also known as physical therapy, is a healthcare profession that specializes in the diagnosis, treatment, and prevention of injuries, disabilities, and disorders affecting the musculoskeletal system. Physiotherapy plays a crucial role in injury recovery, as it helps to restore and improve the physical function and mobility of the affected area.
Home physiotherapy is a type of physiotherapy that is performed in the comfort of one’s own home. There are various types of physiotherapy techniques that can be used in home physiotherapy, depending on the type and severity of the injury.
Some common techniques used in home physiotherapy include:
- Range of motion exercises: These exercises involve moving the affected area in different directions to improve its flexibility and range of motion.
- Strengthening exercises: These exercises help to strengthen the muscles surrounding the affected area, which can help to improve its stability and reduce the risk of reinjury.
- Stretching exercises: These exercises help to improve flexibility and reduce muscle tension, which can help to alleviate pain and stiffness.
- Manual therapy: This technique involves hands-on manipulation of the affected area to help reduce pain, improve mobility, and promote healing.
By using a combination of these techniques, a physiotherapist can create a customized treatment plan tailored to the individual’s specific needs and goals. In the next section, we will explore the benefits of home physiotherapy in more detail.
Benefits of Home Physiotherapy
Home physiotherapy offers numerous benefits that make it a great option for those recovering from an injury. Here are some of the key advantages of home physiotherapy:
- Comfort of familiar surroundings: One of the biggest benefits of home physiotherapy is that it allows you to perform exercises in the comfort of your own home. This can be especially beneficial for those who feel anxious or uncomfortable in a clinical setting.
- Flexibility of scheduling: Home physiotherapy allows for greater flexibility in scheduling. You can work with your physiotherapist to create a schedule that fits your needs and lifestyle, whether that means scheduling sessions before or after work, on weekends, or during lunch breaks.
- Cost-effectiveness compared to in-clinic physiotherapy: Home physiotherapy is often a more cost-effective alternative to in-clinic physiotherapy, as it eliminates the need for travel and facility fees.
In addition to these benefits, home physiotherapy also allows for greater individual attention from a physiotherapist, as they can focus solely on your needs and progress. It also offers a level of privacy that may be preferred by some individuals.
By choosing home physiotherapy, you can take control of your recovery process and work towards achieving your goals in a comfortable and convenient setting.
Preparing for Home Physiotherapy
Before starting home physiotherapy, it is important to properly prepare yourself and your space to ensure that you can perform the exercises safely and effectively. Here are some steps you can take to prepare for home physiotherapy:

- Setting up a designated space for physiotherapy exercises: Designate a specific area in your home where you can perform the exercises comfortably and without interruption. This could be a spare room, a corner of a room, or even a cleared-out space in your garage or backyard.
- Obtaining necessary equipment and tools for the exercises: Depending on the type of exercises your physiotherapist has prescribed, you may need to obtain some equipment or tools to perform them safely and effectively. This could include items such as exercise bands, foam rollers, or weights.
- Finding a qualified physiotherapist to guide you through the process: It is important to work with a qualified and experienced physiotherapist who can guide you through the home physiotherapy process. Your physiotherapist will be able to create a customized treatment plan tailored to your specific needs and goals, as well as monitor your progress and make adjustments as needed.
When looking for a physiotherapist, be sure to choose someone who is licensed and accredited in your area, and who has experience with the type of injury you are recovering from. You may also want to consider factors such as their availability, pricing, and location when choosing a physiotherapist.
By properly preparing yourself and your space for home physiotherapy, you can set yourself up for success and ensure that you are able to perform the exercises safely and effectively.
Common Injuries That Can Be Treated with Home Physiotherapy
Home physiotherapy can be an effective treatment option for a wide range of injuries, from minor sprains and strains to more serious injuries requiring surgery. Here are some common injuries that can be treated with home physiotherapy:
- Sprains and strains: Home physiotherapy can help to reduce pain and stiffness and improve mobility in the affected area. Examples of sprains and strains that can be treated at home include ankle sprains, hamstring strains, and wrist sprains.
- Back pain: Home physiotherapy exercises can help to strengthen the muscles in the back and improve flexibility, which can help to reduce pain and prevent future injuries.
- Post-surgical rehabilitation: Home physiotherapy can be an effective way to recover after surgery, as it allows you to perform exercises in a comfortable and familiar environment. Examples of post-surgical rehabilitation that can be done at home include knee replacement surgery and rotator cuff surgery.
Studies have shown that home physiotherapy can be just as effective as in-clinic physiotherapy for many types of injuries. For example, a study published in the Journal of Bone and Joint Surgery found that home physiotherapy was just as effective as in-clinic physiotherapy for patients recovering from a total knee replacement.
Another study published in the Journal of Orthopaedic & Sports Physical Therapy found that patients who received home physiotherapy for a rotator cuff tear had similar outcomes to those who received in-clinic physiotherapy, with both groups experiencing significant improvements in shoulder function and pain reduction.
Overall, home physiotherapy can be an effective and convenient treatment option for a wide range of injuries, and studies have shown that it can produce significant improvements in pain, mobility, and function.
Home Physiotherapy Exercises
Home physiotherapy involves a variety of exercises and stretches that are designed to improve mobility, strength, and flexibility in the affected area. Here are some common types of exercises and stretches that can be performed at home:

- Range of motion exercises: These exercises involve moving the affected area in different directions to improve its flexibility and range of motion. Examples include shoulder circles, ankle rolls, and wrist bends.
- Strengthening exercises: These exercises help to strengthen the muscles surrounding the affected area, which can help to improve its stability and reduce the risk of reinjury. Examples include squats, lunges, and resistance band exercises.
- Stretching exercises: These exercises help to improve flexibility and reduce muscle tension, which can help to alleviate pain and stiffness. Examples include hamstring stretches, calf stretches, and neck stretches.
When performing home physiotherapy exercises, it is important to start slowly and gradually increase the intensity and duration of the exercises as your body becomes stronger and more flexible. It is also important to work with your physiotherapist to ensure that you are performing the exercises correctly and safely.
Here are some tips for developing and maintaining a consistent exercise routine:
- Set realistic goals: Start with small goals and work your way up. Celebrate each accomplishment along the way, and don’t get discouraged if progress is slow.
- Create a schedule: Set aside specific times each day for your home physiotherapy exercises. This will help you stay on track and make it easier to develop a consistent routine.
- Find an accountability partner: Enlist the help of a friend, family member, or physiotherapist to hold you accountable and provide support and encouragement.
- Mix it up: Try different types of exercises and stretches to keep things interesting and prevent boredom.
By following these tips and consistently performing your home physiotherapy exercises, you can help to speed up the recovery process and improve your overall physical function and mobility.
Monitoring Progress
Monitoring progress is an important part of the home physiotherapy process, as it allows you to track your recovery and make adjustments to your treatment plan as needed. Here are some reasons why monitoring progress is important:
- Identifying areas of improvement: By monitoring progress, you can identify areas where you are making progress and areas where you may need to focus more attention.
- Motivation: Seeing progress can be a powerful motivator and can help you stay on track with your home physiotherapy exercises.
- Making adjustments: If you are not seeing the progress you had hoped for, monitoring can help you and your physiotherapist make adjustments to your treatment plan.
There are several tools and methods you can use to monitor your progress at home, including:
- Keeping a journal: Keeping a journal of your exercises, progress, and any changes in symptoms can help you track your progress over time.
- Taking measurements: Measuring your range of motion, strength, and flexibility regularly can help you see improvements and identify areas where you may need more work.
- Using apps: There are several apps available that can help you track your progress and provide feedback on your exercises.
- Working with a physiotherapist: Your physiotherapist can monitor your progress during each session and make adjustments to your treatment plan as needed.
By monitoring your progress and staying committed to your home physiotherapy exercises, you can maximize your chances of a successful recovery and improve your overall physical function and mobility.
Potential Risks and Precautions
While home physiotherapy can be a safe and effective treatment option for many injuries, there are potential risks associated with performing exercises at home without professional supervision. Here are some potential risks associated with home physiotherapy:
- Reinjury: Without proper guidance, it is possible to perform exercises incorrectly or with too much intensity, which can lead to reinjury.
- Overuse injuries: Overusing the affected area during exercises can lead to pain, inflammation, and other overuse injuries.
- Safety hazards: Performing exercises in an unsafe environment or without proper equipment can lead to accidents or injuries.
To ensure the safety and effectiveness of home physiotherapy, here are some precautions to take:
- Work with a qualified physiotherapist: Working with a qualified and experienced physiotherapist can help to ensure that you are performing exercises correctly and safely.
- Start slowly: Start with low-intensity exercises and gradually increase the intensity and duration as your body becomes stronger and more flexible.
- Use proper equipment and techniques: Use proper equipment and techniques when performing exercises to reduce the risk of injury.
- Listen to your body: Pay attention to how your body feels during and after exercises. If you experience pain or discomfort, stop the exercise and consult with your physiotherapist.
By taking these precautions and working closely with a physiotherapist, you can minimize the risks associated with home physiotherapy and maximize your chances of a successful recovery.
When to Seek Professional Help
While home physiotherapy can be an effective treatment option for many injuries, there may be cases where professional medical attention is necessary. Here are some signs that home physiotherapy may not be enough:
- Pain is getting worse: If your pain is getting worse or is not improving with home physiotherapy, it may be a sign that there is an underlying issue that requires medical attention.
- Loss of mobility: If you are experiencing a loss of mobility or range of motion, it may be a sign that there is an issue that requires medical attention.
- Signs of infection: If you experience signs of infection such as fever, chills, redness, swelling, or pus around the affected area, it is important to seek medical attention immediately.
- Numbness or tingling: If you experience numbness or tingling in the affected area, it may be a sign of nerve damage and requires medical attention.
If you experience any of these signs, it is important to seek the help of a medical professional. A doctor or physiotherapist can assess your condition and determine if additional treatment is necessary. They may recommend additional testing, prescribe medication, or refer you to a specialist for further evaluation.
Remember, it is always better to err on the side of caution and seek medical attention if you have any concerns or questions about your condition.
Conclusion
Home physiotherapy can be a safe, effective, and convenient treatment option for a wide range of injuries. By performing exercises in the comfort of your own home, you can improve your physical function and mobility while avoiding the inconvenience and cost of in-clinic physiotherapy. Here are some of the key benefits of home physiotherapy:
- Comfort of familiar surroundings
- Flexibility of scheduling
- Cost-effectiveness compared to in-clinic physiotherapy
- Customized treatment plans tailored to your specific needs and goals
To ensure the safety and effectiveness of home physiotherapy, it is important to work closely with a qualified physiotherapist, follow proper techniques and precautions, and monitor your progress regularly. Remember, if you experience any signs of worsening pain or mobility, it is important to seek the help of a medical professional.
In conclusion, home physiotherapy can be a great option for those looking to recover from an injury in a comfortable, convenient, and cost-effective manner. By taking the necessary precautions and following your physiotherapist’s advice, you can speed up your recovery and improve your overall physical function and mobility.
The Role of Musculoskeletal Assessment in Enhancing Exercise Performance
Musculoskeletal assessment plays a crucial role in enhancing exercise performance. Not only does it provide valuable information about an individual’s current physical condition but it also helps identify areas of weakness that may be hindering their progress. By identifying these problem areas, trainers and athletes can develop targeted exercise regimens to strengthen these muscles and improve overall fitness.
Additionally, musculoskeletal assessment can help prevent injuries by identifying imbalances or asymmetries that could lead to strain or injury. Through corrective exercises and stretching, athletes can work to address these issues before they become serious problems.
Another benefit of musculoskeletal assessment is the ability to track progress over time. By regularly measuring strength, flexibility, and mobility, individuals can see how far they’ve come and set new goals for continued improvement.
In short, musculoskeletal assessment is a vital tool for anyone looking to enhance their exercise performance. Whether you’re an elite athlete or just starting out on your fitness journey, understanding your body’s strengths and weaknesses is essential for achieving success and avoiding injury.
Common Musculoskeletal Imbalances and Their Impact on Exercise Performance
When it comes to exercise performance, having a well-functioning musculoskeletal system is crucial. Unfortunately, many individuals suffer from common musculoskeletal imbalances that can seriously impact their ability to perform at their best. For example, limited hip mobility can lead to poor squat form and decreased power output during lifts. Tight hamstrings can restrict movement patterns and increase the risk of injury during activities such as running or jumping.
Other common imbalances include weak glutes, tight or weak shoulders, and poor spinal alignment. While these may seem like minor issues, they can have a significant impact on an individual’s overall performance and ability to reach their fitness goals.
Thankfully, by incorporating regular musculoskeletal assessments into one’s fitness routine, these imbalances can be identified and addressed before they become more serious issues. A thorough assessment can help uncover specific areas of weakness or tightness that need to be targeted with corrective exercises or stretches. By doing so, individuals can improve their range of motion, increase strength and power output, and reduce the risk of injury.
In short, taking the time to address common muscle imbalances through regular assessments is key to enhancing exercise performance and achieving optimal results in any fitness journey.
Assessing Musculoskeletal Limitations and Developing Targeted Exercise Programs for Athletes
As a physiotherapist, assessing musculoskeletal limitations and developing targeted exercise programs for athletes is a crucial aspect of my job. Every athlete has unique needs when it comes to their training regime, which is why a one-size-fits-all approach simply won’t do.
By taking the time to carefully evaluate an athlete’s musculoskeletal system, including their posture, range of motion, and muscle strength and flexibility, I can identify any areas of weakness or imbalance that could be holding them back from reaching their full potential. Once these limitations have been identified, I can then develop a customized exercise program that targets these specific areas, helping the athlete to improve their performance on the field or in competition.
Of course, this process is not without its challenges. Athletes often have tight schedules and are constantly pushing themselves to the limit during training and competition. This makes it all the more important for me as a physiotherapist to stay up-to-date with the latest research and techniques in order to provide effective solutions quickly and efficiently.
Ultimately though, seeing an athlete reach new levels of performance thanks to targeted musculoskeletal assessment and exercise programming is incredibly rewarding. Whether it’s helping a football player recover from an injury or giving a gymnast the tools they need to perfect their routine, there’s nothing quite like seeing someone achieve their goals and knowing you played a part in making it happen.
The Importance of Proper Warm-up and Cool-down Techniques in Musculoskeletal Assessment
Proper warm-up and cool-down techniques are integral components of the musculoskeletal assessment process. They play a critical role in enhancing exercise performance, reducing the risk of injury, and improving overall physical health.
During a warm-up, your body increases its core temperature, which helps to improve blood flow to your muscles and joints. This increased blood flow delivers more oxygen and nutrients to your muscles, making them more pliable and ready for exercise. Additionally, a proper warm-up prepares your mind for physical activity by activating mental processes associated with focus and attention.
On the other hand, a cool-down is essential for allowing your body to return to its resting state after exercise. It helps to reduce muscle soreness by promoting the removal of lactic acid from your muscles. Furthermore, it prevents blood pooling in your legs by gradually decreasing your heart rate.
In conclusion, implementing proper warm-up and cool-down techniques as part of the musculoskeletal assessment process is crucial for achieving optimal exercise performance while reducing the risk of injury. Remember: taking care of our bodies before and after exercising is just as important as taking care of them during exercise!
Conclusion
In conclusion, musculoskeletal assessment plays a vital role in enhancing exercise performance for athletes. Identifying common imbalances and limitations can help develop targeted exercise programs that address specific needs for each individual athlete. Proper warm-up and cool-down techniques are also essential to reducing the risk of injury and improving overall performance. By assessing and addressing these musculoskeletal factors, athletes can optimize their training potential and reach peak athletic performance. It is crucial for coaches, trainers, and athletes to prioritize musculoskeletal assessment as they work towards achieving athletic success.
FAQ
What is musculoskeletal assessment?
Musculoskeletal assessment is a process of evaluating an individual’s physical condition, including their posture, range of motion, and muscle strength and flexibility.
How can musculoskeletal assessment enhance exercise performance?
By identifying areas of weakness or imbalance in an individual’s musculoskeletal system, targeted exercise programs can be developed to improve overall fitness and reduce the risk of injury.
What are some common musculoskeletal imbalances that can affect exercise performance?
Common imbalances include limited hip mobility, tight hamstrings, weak glutes, tight or weak shoulders, and poor spinal alignment.
What is the importance of warm-up and cool-down techniques in musculoskeletal assessment?
Proper warm-up and cool-down techniques help reduce the risk of injury and improve overall physical health by preparing the body for exercise and allowing it to return to its resting state after exercise.
Who should prioritize musculoskeletal assessment in their fitness routine?
Coaches, trainers, and athletes should all prioritize musculoskeletal assessment as they work towards achieving athletic success. However, anyone looking to improve their exercise performance can benefit from regular assessments.
Understanding the Link Between Footwear and Foot Pain Relief
When it comes to foot pain relief, footwear plays a crucial role. Poorly fitting shoes can cause a wide range of foot problems, including blisters, calluses, corns, and even serious medical conditions like plantar fasciitis and heel spurs.
Understanding the link between footwear and foot pain relief requires some basic knowledge about what makes a good shoe. First and foremost, the shoe should fit properly – meaning it’s not too tight or too loose. It should also provide ample arch support to help distribute your weight evenly across your feet. This can help prevent strain and overuse injuries that often lead to chronic pain.
Selecting the right type of shoe is also essential for foot pain relief. For example, individuals with flat feet may benefit from shoes with more rigid soles to help maintain proper alignment. Athletes or those who engage in high-impact activities may require shoes with extra cushioning to absorb shock.
Overall, investing in high-quality footwear that offers proper support and fits well is one of the most effective ways to alleviate foot pain. So don’t neglect your feet – treat them well with comfortable shoes that will keep you moving pain-free!
The Importance of Proper Arch Support in Footwear for Pain Relief
When it comes to foot pain relief, proper arch support in footwear is essential. The arch of your foot plays a critical role in maintaining balance and distributing weight evenly across your feet when walking or standing. Sadly, most shoes on the market lack adequate arch support, leading to various foot conditions such as plantar fasciitis, heel spurs, and bunions.
The importance of proper arch support in footwear cannot be overstated. Choosing the right pair of shoes with sturdy and supportive arches can make all the difference in reducing and preventing pain. These shoes help stabilize the foot, promote better posture, and reduce pressure on sensitive areas such as the heel and ball of your foot.
Additionally, inadequate arch support puts unnecessary strain on your feet’ ligaments, bones, nerves and muscles leading to discomfort or injury over time. Therefore investing in high-quality shoes with the right amount of arch support can help you walk or stand for extended periods without feeling tired or achy.
In conclusion, choosing proper footwear with suitable arch support is crucial for optimal foot health and pain relief. Not only will it provide much-needed comfort but prevent future complications that may require long term medical attention. So next time you buy a new pair of shoes put aside style considerations; instead prioritize functionality by finding one that provides excellent arch support for maximum relief.
The Role of Cushioning and Shock Absorption in Footwear for Pain Management
If you suffer from foot pain, you likely already know that investing in good, supportive footwear is key to finding relief. But did you know that the role of cushioning and shock absorption in your shoes can make a big difference in managing your pain?
Cushioning refers to the soft, spongy material inside your shoe that helps absorb impact with each step. This can be especially important if you have conditions like plantar fasciitis or heel spurs, which can cause pain with each step.
Similarly, shock absorption helps reduce the amount of force transmitted through your foot when you land while walking or running. This can help protect your joints and reduce overall wear and tear on your feet.
But it’s not just about having more cushioning or better shock absorption; it’s about finding the right balance for your specific needs. Too much cushioning can actually lead to instability and increased risk of injury. That’s why it’s important to work with a knowledgeable professional – like a podiatrist or trained shoe fitter – to find shoes that provide the right level of support for your individual situation.
Ultimately, investing in good shoes with proper cushioning and shock absorption is essential for managing foot pain over the long-term. So don’t skimp on this important aspect of self-care – your feet (and overall well-being) will thank you!
The Benefits of Wearing Orthotic Inserts for Foot Pain Relief
Are you one of the many people who suffer from chronic foot pain? Perhaps you’ve tried various types of footwear and have yet to find relief. Well, let me tell you about the benefits of wearing orthotic inserts for foot pain relief.
Orthotic inserts are designed to provide support and cushioning to the feet in order to alleviate various types of foot pain. They can be used to treat conditions such as plantar fasciitis, flat feet, high arches, and more.
One of the key benefits of orthotic inserts is that they can help redistribute pressure on your feet. This helps reduce stress on certain areas that may be causing pain or discomfort. Additionally, orthotic inserts can help improve biomechanical alignment, which can also reduce strain on your feet and improve overall comfort.
Another benefit of orthotic inserts is that they can be tailored to your individual needs. Custom-made orthotics are designed specifically for your feet, taking into account factors such as foot shape and gait pattern. This personalized approach means that you’re more likely to find the right level of support and cushioning needed for your unique condition.
So if you’re tired of struggling with foot pain and want a solution that truly works, consider investing in a pair of orthotic inserts. Your feet (and entire body) will thank you!
How to Choose the Right Shoes for Your Foot Type to Alleviate Pain
When it comes to selecting the right pair of shoes, many people go for style over comfort. However, ignoring the importance of foot type can lead to discomfort and even pain in the long run. Each foot is unique with different arches, widths, and sizes. Understanding your foot type is crucial to avoid unnecessary suffering.
Flat feet have low or no arches and require more support to prevent foot fatigue and pain. They need shoes with extra cushioning on the sole to absorb shock while walking or running. High arches, on the other hand, require shoes with more flexibility that won’t put too much pressure on them.
Wide feet need plenty of space in the toe area as well as a wider width size while narrow feet need shoes with snug fitting that prevent them from moving around.
In summary, choosing the right shoes for your foot type can alleviate existing pains or prevent them from happening in the future. Don’t hesitate to seek professional advice if you’re unsure about your foot type or shoe selection. Remember that happy feet make for a happy body!
Conclusion
In conclusion, wearing proper footwear is crucial for managing foot pain and providing relief. The importance of arch support cannot be overstated, as it helps to distribute pressure evenly across the foot and reduce strain on the plantar fascia. Additionally, cushioning and shock absorption play a vital role in preventing impact-related injuries and reducing discomfort while walking or standing for extended periods. Those suffering from foot pain may also benefit from orthotic inserts designed to provide personalized support that can alleviate pain and prevent further injury. Finally, understanding your foot type is critical when selecting shoes to ensure that you are choosing footwear that will provide the right level of support and comfort for your needs. By following these guidelines, individuals can choose the right footwear to alleviate existing pain and prevent future foot-related issues.
FAQ
Can wearing high heels cause foot pain?
Yes, wearing high heels can cause foot pain. They put stress on the feet and can lead to conditions like plantar fasciitis, as well as blisters and calluses.
Are flip flops bad for your feet?
Flip flops lack proper arch support and cushioning, which can lead to foot pain over time. They are not recommended for daily wear or activities that require extended standing or walking.
Can I use over-the-counter orthotics instead of custom-made ones?
Over-the-counter orthotics may provide some relief but they cannot offer the same level of customization as custom-made orthotics. If you have a specific foot condition or need tailored support, it’s best to consult with a podiatrist or trained shoe fitter and get a personalized solution.
How often should I replace my shoes for foot pain relief?
It depends on how frequently you wear them and the type of activity you engage in. As a general rule, most shoes should be replaced every 6-8 months with regular use. However, if you notice signs of excessive wear or discomfort sooner than that, it may be time to replace them earlier.
Can I still exercise with foot pain?
Depending on the severity and type of foot pain, it may be possible to continue exercising with modifications to your routine or equipment. However, it’s important to consult with a medical professional before continuing any physical activity while experiencing foot pain to avoid exacerbating the condition.
5 Surprising Ways Pelvic Floor Physiotherapy Can Benefit Postpartum Women in Edmonton
Being a mom is an incredible journey but it’s important to ensure that any physical changes brought about by pregnancy and childbirth aren’t ignored. Among the many benefits of pelvic floor physiotherapy, there are five surprising ways that postpartum women in Edmonton can benefit from this specific type of treatment.
Firstly, pelvic floor physiotherapy can help with urinary incontinence or leakage. Many women experience this issue after childbirth due to weakened muscles in the pelvic floor, which can be treated effectively by a qualified physiotherapist.
Secondly, pelvic pain and discomfort can also be alleviated through physiotherapy. This pain could be caused by healing muscles, scar tissue or nerve damage post-birth – all of which can be addressed with specific therapies.
Thirdly, if you’ve experienced painful intercourse since giving birth, pelvic floor physiotherapy may offer relief. With vaginal manipulation techniques and exercises designed to strengthen tissues, sex doesn’t have to hurt after having a baby.
Fourth on our list – did you know that some postpartum women experience constipation issues? Pelvic floor therapy can improve bowel function by strengthening the same muscles used to control urinary flow (which is why something as simple as Kegel exercises are so beneficial!).
Lastly (but certainly not least), many new moms find themselves experiencing postpartum depression, anxiety or PTSD. While depression or anxiety requires more than just physical therapies, research has shown that rehabilitation for weak pelvic-floor muscles leads to improvements in mental health too.
If you’re struggling with any of these challenges post-childbirth or simply want to prioritize your overall health during this transformative time in your life – reach out to the team at our clinic today! Taking care of yourself is always worth it.
How Pelvic Floor Physiotherapy Helps Improve Bladder Control After Pregnancy
Pelvic floor physiotherapy is a powerful tool that can help new mothers regain control over their bladder, which may have been weakened during pregnancy or childbirth. The pelvic floor muscles are responsible for supporting the bladder, and if they become damaged or weak, it can result in leaking urine or even incontinence.
Pelvic floor physiotherapy works by targeting these muscles to help restore strength and function. A trained physiotherapist will work with the mother to identify any areas of weakness or tension in the pelvic region, and develop a customized treatment plan that includes exercises, stretches, and other techniques to promote healing.
In addition to improving bladder control, pelvic floor physiotherapy can also help alleviate pain and discomfort associated with pregnancy and childbirth. This can include back pain, hip pain, groin pain, and more.
So if you’re a new mother struggling with bladder control issues after pregnancy or childbirth, consider giving pelvic floor physiotherapy a try. With the right treatment plan and guidance from a skilled professional, you can take control of your health and get back to feeling like yourself again in no time!
The Role of Pelvic Floor in Postpartum Recovery: Understanding the Importance
Pregnancy and childbirth can cause a significant impact on a woman’s pelvic floor muscles. The pelvic floor is a group of muscles that support the uterus, bladder, bowel, and rectum. During pregnancy and childbirth, these muscles stretch to accommodate the growing baby and facilitate its passage through the birth canal.
The pelvic floor plays an essential role in postpartum recovery. It helps control urinary incontinence, sexual function, and core stability. Unfortunately, many new mothers experience issues with their pelvic floor muscles after giving birth. These problems can include incontinence, discomfort during sex, pelvic organ prolapse, and back pain.
Pelvic Floor Physiotherapy is an effective way to address these issues for new mothers. By working with a Pelvic Floor Physiotherapist in Edmonton postpartum women can learn exercises that will help them regain control of their pelvic floor muscles. These exercises may involve strengthening the pelvic floor or learning how to relax these muscles properly.
There are also other surprising ways that Pelvic Floor Physiotherapy can benefit postpartum women:
1) Improved core stability- A weak pelvic floor can lead to back pain as well as instability around the trunk region. Pelvic Floor Physiotherapy strengthens your core which leads to better balance and a stronger lower-back.
2) Reduce Risk of Future Issues – Strengthening the pelvic floor after giving birth not only addresses current problems but reduces future risks such as incontinence or prolapse down the line.
3) Better Bladder Control- Urinary incontinence is a common problem among new mothers due to weakened pelvic floor muscles; however, this issue can be resolved by working with a physiotherapist who specializes in connecting those internal structures with external cues for greater bladder control.
4) Enhanced Sexual Function – Pelvic Floor Physiotherapy can help improve sexual function by ensuring proper muscle contraction easing discomfort related to intercourse.
5)Reduced Pain – Physical therapy can help relieve pain associated with issues related to the pelvic floor muscles
Addressing Sexual Dysfunction in Postpartum Women: The Benefits of Pelvic Floor Therapy
Postpartum women often face sexual dysfunction, which can be a major concern for many new mothers. Thankfully, pelvic floor therapy can provide a multitude of benefits that can help alleviate these concerns.
First and foremost, pelvic floor therapy helps to strengthen the muscles of the pelvic floor. This is important because weak or damaged muscles in this area can lead to urinary and fecal incontinence, as well as pain during intercourse. By strengthening these muscles, pelvic floor therapy can provide significant relief for postpartum women.
Additionally, pelvic floor therapy can help with scar tissue and adhesions that may have been left behind from delivery. This often goes unnoticed by medical professionals but can lead to painful intercourse or general discomfort in daily life.
Incorporating pelvic floor therapy into postpartum care plans also helps women embrace their sexual health without judgment or stigma. Many women feel overlooked after childbirth when all attention turns towards the baby’s well-being while neglecting the mother’s needs. By giving women an opportunity to talk openly about sexual dysfunction with a professional who specializes in this subject matter, confidence and self-worth are restored.
Lastly, engaging in physical touch has proven health benefits. It helps with relaxation and stress-relief as it triggers our brain’s innate ability to release oxytocin (feel-good hormone). Pelvic floor physiotherapy provides an ultimately positive space where patients experience safe touch with a professional they trust.
Overall, addressing sexual dysfunction through pelvic floor therapy is just one of many ways postpartum women benefit from specialized care following childbirth. So if you’re experiencing any discomfort or pain during sex after having a child and need expert guidance in reclaiming your sex life again confidently – book an appointment today!
Conclusion
In conclusion, pelvic floor physiotherapy offers numerous benefits for postpartum women in Edmonton. It can improve bladder control, which is often compromised after pregnancy and childbirth. The pelvic floor plays a significant role in postpartum recovery, so it’s important to understand its importance and seek therapy if necessary. Additionally, pelvic floor physiotherapy can address sexual dysfunction in postpartum women, helping them get back to enjoying an active sex life. Overall, by seeking out the services of a skilled pelvic floor physiotherapist, new mothers can experience improved quality of life and increased confidence in their physical abilities.
FAQ
Can pelvic floor physiotherapy benefit women who have never given birth?
Yes, absolutely! Pelvic floor dysfunction can affect women of all ages and backgrounds, not just postpartum women. Pelvic floor physiotherapy can help improve bladder control, alleviate pain and discomfort during sex, and address other issues related to weakened or damaged pelvic floor muscles.
Is there a specific time frame for postpartum women to start pelvic floor physiotherapy?
It’s recommended to wait until after your six-week postpartum checkup before starting any physical therapy. However, if you’re experiencing significant pain or discomfort before then, it’s important to speak with a healthcare provider about possible next steps.
What should I expect during my first pelvic floor physiotherapy appointment?
During your first appointment, the therapist will likely ask you questions about your medical history and any symptoms you’re experiencing. They may also perform a physical exam to assess the strength and function of your pelvic floor muscles.
How many sessions of pelvic floor physiotherapy will I need?
The number of sessions needed varies depending on the individual’s condition and treatment goals. Some patients see improvements after just a few sessions while others may require several weeks or months of therapy. Your physiotherapist can give you a better understanding of what to expect during your initial visit.
Are there any risks associated with pelvic floor physiotherapy?
Generally speaking, pelvic floor physiotherapy is very safe and poses minimal risks. However, as with any type of physical therapy or medical treatment, there is always a slight risk of injury or exacerbation of existing symptoms. It’s important to work with a qualified and experienced professional who can help minimize these risks and keep you safe throughout the course of treatment.










